Christian Healthcare Ministries Maternity Program Review
HOW TO PAY FOR YOUR PREGNANCY AND BIRTH WITHOUT HEALTH INSURANCE
Hi there, I’m Katie Jones, a Certified Christian Financial Counselor, and I have been a CHM member for about 4 years. I have had a lot of experience being a part of CHM, including knee surgery, an ambulance run for my husband resulting in an ankle surgery for him, and most recently a pregnancy!
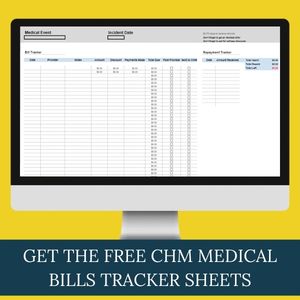
I have previously shared my overall review of Christian Healthcare Ministries as well as shared some tips on How to Manage Bills as a CHM member, and specifically How to Submit Bills to CHM.
If you are not already a part of CHM and are considering it, I would greatly appreciate you considering using our family referral link to sign up. We do receive a kickback from CHM, so thank you in advance for your support!
All information is subject to change! I created this in early 2024. Please always consult the CHM Guidelines or connect with the CHM Maternity Support Team through email or phone if you have further questions.
Okay, so this video is pretty long, so if you have a specific question you are looking to get answered, go down to the description below and click on the chapter that you want to hear the answer to.
What is Christian Healthcare Ministries?
Christian Healthcare Ministries is a health cost-sharing ministry. It replaces traditional health insurance, though it is not health insurance itself.
I have a full review of CHM and compare it to other cost-sharing ministries if you’d like to learn more about CHM as a whole. If you are a CHM member an need help with how to manage your medical bills be sure to check out my video on how I do that for our bills.
In this article, I specifically want to share my experience with CHM’s maternity program.
My Review of the CHM Maternity Program
Overall, I had a pretty good experience with the CHM Maternity Program, up until I had some complications with my labor. But let me explain further before you panic.
It was extremely simple to navigate the CHM Maternity Program once I got pregnant. In a nutshell, this is the process to getting your maternity bills shared:
- Call CHM to let them know your pregnant
- Pick a provider
- Receive your Global Fee from the provider and submit it to CHM
- Wait to receive your Global Fee reimbursement from CHM (around 30 weeks)
- Pay your provider
- Have your baby!
- Submit any other maternity-related bills to CHM (this is also ongoing during pregnancy)
Now, the thing that I “messed up” on was the fact that my husband and I were NOT a part of the CHM Plus Program (formerly known as the Bother’s Keeper Program). This would not have been an issue at all, except that my baby and I ended up getting very ill from an infection during labor. We were hospitalized for a month and between the two of us incurred roughly $3 million in medical bills (before discounts).
With CHM+ we would not have had any issues with getting our medical bills shared amongst the ministry, however, that was not the case.
Thankfully, we learned that we qualified for Medicaid and we were able to have all of our hospital-related medical expenses shared with no issues. Though it did take about 45 days to be approved and it was a little stressful in the meantime waiting to hear if we would be shared or not.
In the end, we didn’t have any out-of-pocket medical expenses for the pregnancy and birth except for a few small things in the beginning that CHM did not share. We also would not have had any expenses out of pocket besides those few things if we had no complications as well. If I could go back and change one thing it would be to add CHM Plus to our membership before becoming pregnant; I highly recommend it.
How to Get CHM Maternity Questions Answered
The CHM Maternity Program does have its own support line and email address: Maternity@chministries.org
If you do still have any questions about the CHM Maternity Program after reading this article please feel free to ask them in the comments. I would be happy to help if I can, or at least guide you in the right direction.
CHM Maternity Facebook Group
CHM has a Facebook group specifically dedicated to the maternity program. Many of the questions I answer here are answered with the help of some of the CHM members in this Facebook group.
This is the description of the CHM Maternity Program group:
This is a private group for members who are currently using, have used in the past, or are interested in our Gold level’s maternity sharing assistance.
This space is intended to be a place of support and prayer. CHM staff members are always available to answer any questions that arise.
CHM is a ministry, first and foremost. Feel free to share your prayer requests with us. To get started, please read and agree to the group rules. Thank you for being here.
There are women asking questions in this group that I never even considered until I came across them in the feed. You will also be able to read other CHM Maternity Program reviews and experiences.
I highly recommend jumping in and asking your questions there to hear about the experiences of other mamas with their maternity-related expenses.
Maternity Sharing Qualifications
To qualify for maternity sharing in Christian Healthcare Ministries, a CHM member must meet the following criteria:
- The member must be married at the time of conception
- The member must be a CHM member for at least 300 days prior to the expected due date. The due date is to be verified by a physician or midwife.
If you do not meet these two requirements, unfortunately, the entire maternity event is ineligible for sharing.
It should also be noted that the pregnancy cannot be a result of IVF, embryo implants, or transfers. This makes the maternity event ineligible as well.
Learn more about maternity eligibility in the CHM Guidelines.
Does CHM Have “In-Network” Providers?
This is one of the BEST things about Christian Healthcare Ministries – they DO NOT have In-Network providers, which means that you can choose whomever you prefer for your pregnancy and birth. You can choose a home birth, birth center, or hospital. This is what really sets CHM apart from not only traditional health insurance, but also apart from other health cost sharing programs such as Medishare; which does have “In-Network” providers.
How Much Does Maternity Cost With CHM?
CHM will share pretty much every maternity-related expense with a few exceptions listed later. You will still have a Personal Responsibility (similar to a deductible) which is based on your program level (visit CHMinistries.org/programs for details). The Maternity Personal Responsibility is per pregnancy and is separate from the annual Personal Responsibility for other medical incidents throughout the year. This is the amount that a CHM member is responsible for paying before their maternity costs can be considered for sharing.
You can receive a $500 credit toward your Personal Responsibility no matter what program you are a part of in the following way:
Members must contact the Maternity Support Team by phone within the first 16 weeks of pregnancy @ 1-800-791-6225 and select Maternity. Keep reading to learn how this initial phone call went for me.
You should also be aware that you have 6 months from the date of any services provided to submit bills to CHM to be considered for sharing. This gives you some time to get settled in to your routine with a new baby before needing to get any other medical bills submitted.
Learn more about the Maternity Personal Responsibility in the CHM Guidelines (CHMinistries.org/guidelines).
Initial Maternity Care Team Contact
Once I found out that I was pregnant, I gave the CHM Maternity Care Team a call to let them know. They first said congratulations (I appreciated the personal congratulations) and asked me questions to verify that I met the qualifications as mentioned previously.
These are the questions they asked me:
- Where I planned to deliver, who my doctor would be, and their address
- I didn’t have exact info yet, so I gave them the name of the birth center we were considering at the moment. Obviously, I didn’t know who the midwife would be so they just told me to let them know once I knew.
- Did I have any current complications
- Didn’t know if I had any yet at 5 weeks pregnant either. They told me to let them know if any came up along the way.
- What number pregnancy was this for us
- This also included any potential miscarriages, of which I have had none. So this was our first pregnancy.
- If the baby was conceived through IVF or IUI
- This answer was a no for us. Maternity events resulting from IVF and certain IUI procedures are not eligible for sharing. (There are times that CHM can share for pregnancies resulting from an IUI procedure when the sperm belonged to the husband. IUI procedure itself and any associated treatments are not eligible.)
The woman on the phone did not specifically ask me if the baby was conceived out of wedlock, but I did start our conversation out by saying “my husband and I found out that we are pregnant” so this probably covered that question.
Then they reminded me to ask our provider for a global fee and to submit it to CHM as soon as I received it. They also reminded me to send in any other itemized bills as they happened.
Check out this video on how to submit a bill to CHM if you haven’t ever done that before.
They also told me to reach out to the Maternity Nurse Navigator, Caitlyn, if I needed any help with non-emergency pregnancy and birth-related questions.
She let me know that I would be receiving an email with all of this information as well as a confirmation that the $500 Personal Responsibility credit was applied to my account.
CHM Maternity Confirmation Email
Just as stated on the phone, I received an email with all the important information from our phone call plus a confirmation that the $500 Personal Responsibility credit was applied to my account and what date it was applied.
*Please note that the Personal Responsibility amount has changed since I received this email.
The Maternity Global Fee
What is a Global Fee?
A maternity global fee, also known as global maternity care or total maternity care, is a complete one-time billing structure that shares all professional services related to maternity care. This includes prenatal care, delivery, and postpartum care, but typically does not include the first visit to your provider to confirm your pregnancy.
You must request a global fee from your provider and submit it to CHM as soon as you receive it. Typically, your provider will give you the global fee and it will have a due date on it or you will need to make monthly payments. Sometimes there is a discount for paying it early. Double check that the global fee has all the CPT codes listed for each service before submitting it to CHM.
In my case, I was able to let my birth center know that our health cost-sharing ministry would be paying us around week 30 and that we would be able to pay everything once we received that. They made the note in my chart and there were no issues.
When Does CHM Send The Reimbursement for the Global Fee?
I have been told that if sent in ASAP to CHM, you should expect to receive the check in the mail from them around 30 weeks.
In our case, we received it right before week 30. I simply let the birth center we were going to know that we were waiting for that check and then we would pay the amount in full. By paying the amount in full they offered a larger discount as well. They made a note in their system and had no issues with that.
Maternity Expenses
What Maternity Expenses Are Shareable?
Note: If a maternity event is determined ineligible, then any services listed or complications related to the pregnancy and delivery for both mother and baby are also ineligible.
Eligible Pregnancy Expenses
The CHM Guidelines (CHMinistries.org/guidelines) and CHM’s Maternity Guide (CHMinistries.org/blog/maternity) includes an up-to-date detailed list of eligible expenses.
In my experience with CHM, these types of medical expenses were eligible for sharing while I was pregnant. I highly recommend looking at the current list of eligible expenses in CHM’s Maternity Guide.
a. Obstetricians or legally practicing midwives—CHM shares bills from either
1) one obstetrician, -or-
2) one midwife (including one assistant at birth or delivery).
b. Prenatal visits.
c. Ultrasounds—up to three, provided they’re medically necessary. More than three will be evaluated on a case-by-case basis, and medical records may be required. Nuchal translucency ultrasounds are not eligible for sharing.
d. Immunizations related to the mother’s prenatal care.
e. Maternity-related prescription medications.
f. Labor and delivery facility charges for mother and baby—include hospital facilities, birthing centers, and home births.
g. Complications for mother and baby.
Eligible Genetic Testing
a. Must be non-invasive and required to determine treatment for a current medical condition.
b. Medical records or healthcare provider notes are required for verification.
c. An amniocentesis may be considered for sharing when medical records confirm that the procedure is necessary to determine life-preserving medical care for baby and/or mother.
Eligible Postnatal Care
Postnatal care for an eligible maternity event can be considered for sharing according to the following criteria:
a) Expenses must be incurred within 90 days of delivery/birth.
b) Mother must stay active on CHM Gold throughout the entire sharing process.
1) Postpartum visits
2) Lactation consultations (after delivery) as needed
3) Baby well visits and problem-focused visits
4) Circumcision for baby
5) Cheek/lip/tongue tie correction for baby
6) Postpartum depression treatment—sharing can include inpatient treatment, counseling, prescription medications, and follow-up care as needed. Medical records may be requested to confirm the postpartum diagnosis. This is also available for women experiencing loss through miscarriage or stillbirth.
7) Expenses for a miscarriage or stillbirth can be considered for sharing even if the pregnancy wasn’t eligible for sharing
8) Pelvic Floor Therapy for 90 days after delivery. You have up to 45 visits.
Should you need continued visits that extend passed the initial 90 days (If you have not reached the 45 visit limit yet) after delivery – they will be separated from the Maternity Event and placed under their own incident to be processed with Regular Sharing. Please Note: If that were to be the case, Regular Sharing has a Personal Responsibility of $1000 per calendar year that would need to be assessed out of those bills.
Ineligible Maternity-Related Expenses
The CHM Guidelines includes a list of eligible and ineligible maternity expenses. You can download the Guidelines right from the CHM website, CHMinistries.org/guidelines.
CHM also has a Maternity Guide which includes details about their maternity program, including what expenses are eligible. The Maternity Guide is found here: CHMinistries.org/blog/maternity.
At the time of my pregnancy, these were some of the expenses that were not eligible for sharing.
- Pregnancies for unwed mothers. This applies to expenses incurred for the baby’s birth including the initial hospital bills for the baby.
- Contraceptives or birth control
- Over-the-counter medications
- Doula services
- Breast pumps – this is only slightly annoying with the understanding that if you had traditional insurance, under the Affordable Cares Act you are entitled to receive a free breast pump. You can apply to receive WIC benefits and they offer free breast pumps, or connect with your hospital to see if they offer free pumps. Otherwise, some cheaper options would be to rent your pump or find one used
- Fertility procedures or treatments
- Gestation or surrogate maternity procedures
- In vitro fertilization (IVF) and maternity expenses or complications resulting from IVF. This applies to expenses incurred for the baby’s birth, including the initial hospital bills for the baby.
- Sperm donation and pregnancy as a result of sperm donation
- Embryo implants, transfers, or adoptions and maternity expenses or complications resulting from such procedures
- Tubal ligations, vasectomies, or reversal procedures
- Invasive genetic testing such as amniocentesis, chorionic villus sampling, or nuchal translucency ultrasound – A woman in the Facebook Group said it was around $250 to do a NIPT Test out of pocket
- Travel expenses for members, midwives, or any other inidividuals
- Charges for baby’s care during and immediately following delivery (prior to discharge) when part of an ineligible maternity event
- Unnecessary ultrasounds – Ask your provider how they label and bill your 20-week ultrasound. CHM will not share the expense if it is billed as a “Gender Reveal Ultrasound” instead of an Anatomy Ultrasound
- Postnatal vaccinations/immunizations are ineligible for both mother and baby – I recommend going to your local Department of Public Health to get discounted or even free vaccines for you and your baby.
Services related to congenital birth defects must be shared under the baby’s unit and cannot be included in the maternity event.
Any treatments that take place more than 90 days from delivery/birth must be processed as a new medical incident independent of the maternity event. As with any new medical incident, Personal Responsibility and Qualifying Amount per incident must be met.
What Does CHM Share for Home Births?
If you go back and look at the list of eligible expenses, a home birth is listed there. The needs for a homebirth are going to be different than being in a facility since all of the supplies and materials will need to be purchased.
One mama in the CHM Maternity Facebook Group said this:
“They told me my birth kit would be covered as long as it was clear it was from a birthing site and it was a birth kit requested by my midwife. Same for the birth pool. So like nothing from Amazon. “
Another mama recommended the site In His Hands Birth Supply and said that CHM shared all the expenses except for the shipping costs. She purchased the whole kit which included the tub, liners, hose, net, thermometer, pumps, and more.
I believe you will need to submit a letter from you midwife stating which supplies they are requesting you purchase.
How Does CHM Share the Costs for Twins?
A mama in the Facebook Group said this:
I just had my twins 13 weeks early and everything has been covered, including the increased visits and the NICU stay for them both! They didn’t have a necessity for major surgeries or anything though so that is something I’m not sure about
A CHM staff member also said in the Facebook Group, that twins are eligible for sharing, and that they’ll just ask that you upload a Letter of Explanation letting them know as you submit your medical bills. Both twins’ expenses are eligible for sharing under the mom’s program for 30 days just like any other baby.
Does CHM Share Expenses for Lactation Consultations?
Lactation consultations are only eligible for sharing after delivery.
One mama in the Facebook Group said that CHM shared a lactation consultation from when she was still in the hospital as well as afterward, but that she needed to send in a referral from her doctor to prove that the consultation was necessary.
It is my understanding that as long as they are considered “necessary” there is no limit to the amount of consultations CHM will share.
Does CHM Share the Costs Of Labor and Birth Complications?
The short answer is yes!
They will share the costs for ambulance transfers if you are doing a home birth or a birth center birth and need to transfer to a hospital due to a complication. CHM may require your midwife or doula to write a letter of explanation as to why the hospital transfer was necessary and what the complication was.
I would also recommend that if you are not yet pregnant, you make sure you are on the CHM+ program so that all of your medical bills are shareable if they exceed the maximum sharing amount.
What Happens If I Have a Miscarriage?
Medical expenses incurred during a miscarriage or stillbirth are eligible for sharing even if the maternity event is not eligible. CHM cannot share these expenses if the member is in violation of membership qualifications.
Miscarriages and stillbirths will be processed as a medical incident, not a maternity event. Therefore, the bills will be processed according to the member’s participation program; the respective Qualifying Amount per incident Personal Responsibility will apply.
What If You Need to Change Providers Mid-Pregnancy?
You will need to send in a Letter of Explanation to CHM as to why you made the switch, but when I asked about it on the phone they made it sound like it was no big deal if I needed to do that.
If you change providers before delivery you must submit a final itemized bill from the original provider and an itemized bill for the new provider. If funds have already been shared, the member must return any over-shared amounts or CHM will pro-rate sharing for the new provider accordingly. If you did pay your previous provider the global fee and switched afterwards, you will need to acquire a refund receipt from them and submit that to CHM before they can provide any other needed funds for the new provider you choose.
This technically happened to me when I needed to be transferred from my birth center to the hospital to give birth to my baby after a few complications arose.
At What Point Does Baby Need Their Own CHM Membership?
Your baby will be on your maternity plan for 30 days. You will need to contact CHM within those first 30 days to get them set up with their own membership. They will need the baby’s full name, date of birth, social security number, and the program you would like them on.
Something cool about CHM is that all children are considered 1 unit. So if you have 2 kiddos, they are considered one unit. Therefore, you will only pay for 3 memberships- yours, your spouse’s, and your kiddos.
Conclusion – CHM Maternity Program Review
Overall, I really enjoyed CHM’s Maternity Program and am thankful that CHM does not have an “in-network” list of providers that you need to use. This gave us the chance to pick whom ever we wanted to be our provider. The main thing I would do differently if I could go back in time is to add the CHM+ program to our membership.
I hope this covers most of your questions about the Maternity Program at Christian Healthcare Ministries. If you do have more questions feel free to drop them in the comments and I will do my best to answer them or point you in the direction of how to get them answered!



